Can’t Sleep? These 7 Research-Backed Techniques for Insomnia Actually Work
Start experimenting with one or two of these to start finding out what works for you
INSOMNIA
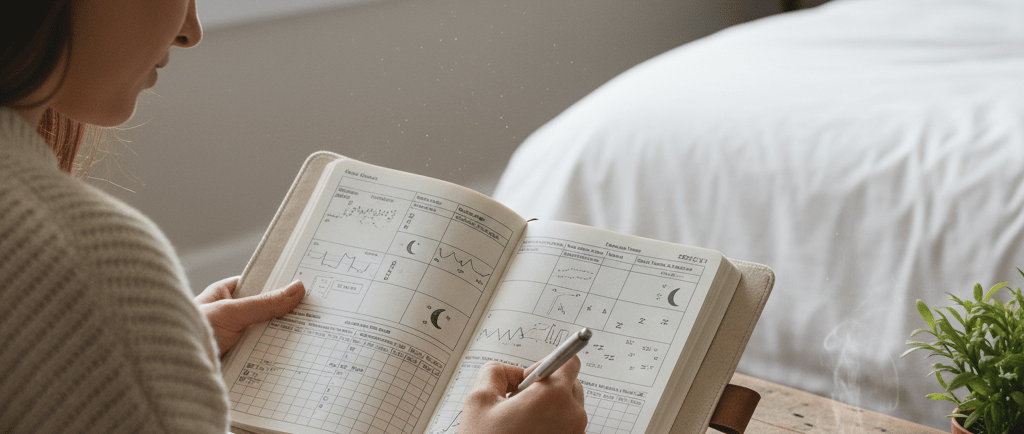

You can power through deadlines, presentations, and tough conversations—but when it comes to sleep, willpower doesn’t work. The harder you try to shut your brain off at night, the more it seems to resist. For many working professionals, this creates a frustrating cycle: late nights of tossing and turning, mornings that start with exhaustion, and days filled with caffeine just to stay afloat.
Take Maya, for example—a 32-year-old project manager who came to therapy saying, “I can handle back-to-back client meetings, but lying in bed at night feels impossible. I just keep thinking about the next day’s emails.” Maya’s story is not unique. In fact, chronic insomnia affects about 10–15% of adults, and it’s especially common in busy professionals managing stress, screens, and irregular schedules (Morin et al., 2021).
The good news is that you don’t have to stay stuck in this cycle. Cognitive Behavioral Therapy for Insomnia (CBT-i) is considered the gold standard treatment for chronic insomnia—often more effective than sleep medication, and with longer-lasting results (Trauer et al., 2015). Let’s walk through seven proven CBT-i techniques, using Maya’s journey as a guide.
1. Sleep Restriction Therapy (SRT)
What It Is
Sleep Restriction Therapy limits your time in bed to closely match the amount of time you’re actually sleeping. Over time, this builds sleep pressure—essentially re-training your brain to fall asleep more quickly and stay asleep.
Research Insight
Studies consistently show that SRT is one of the most powerful components of CBT-i. In a meta-analysis, it was shown to improve sleep efficiency (the ratio of time asleep vs. time in bed) by as much as 15–20% (Kyle et al., 2014).
Maya’s Example
When Maya began CBT-i, she reported going to bed at 10:00 p.m. but not falling asleep until close to midnight. She was spending 8.5 hours in bed but only sleeping about 6. To start, we “restricted” her bedtime to midnight, setting her wake-up for 6:00 a.m. Within two weeks, her brain began linking bed with sleep rather than frustration.
2. Stimulus Control
What It Is
Stimulus control strengthens the mental association between bed and sleep. The rule is simple: bed is for sleep and intimacy only. If you’re awake for more than 15–20 minutes, get up and do something calming until you feel sleepy again.
Research Insight
This technique dates back to Bootzin (1972) and remains a core element of CBT-i. It helps break the cycle of “conditioned arousal”—when the bed becomes associated with wakefulness, worry, or even dread.
Maya’s Example
Instead of lying in bed replaying conversations from the day, Maya started keeping a book of poetry by her couch. If she couldn’t sleep, she’d quietly read until drowsy. Within a month, her anxiety about bedtime significantly decreased.
3. Cognitive Restructuring
What It Is
At the core of CBT-i is addressing the unhelpful thoughts that fuel insomnia. These include catastrophic beliefs (“If I don’t sleep, tomorrow will be a disaster”) or rigid rules (“I must get 8 hours every night”). Cognitive restructuring challenges these beliefs and replaces them with more balanced perspectives.
Research Insight
Harvey et al. (2011) found that dysfunctional sleep beliefs strongly predict insomnia severity. Changing these beliefs reduces not only nighttime anxiety but also daytime fatigue.
Maya’s Example
Maya often thought, “If I don’t sleep at least 7 hours, I’ll completely fail tomorrow’s presentation.” Together, we explored evidence from her own experience: she’d often delivered well on 5–6 hours of rest. This reframing reduced her panic and helped her approach sleep with more calm.
4. Sleep Hygiene (With Nuance)
What It Is
Sleep hygiene refers to lifestyle habits that support healthy sleep—things like reducing caffeine, limiting late-night screen use, and creating wind-down rituals.
Research Insight
On its own, sleep hygiene is rarely enough to treat chronic insomnia (Stepanski & Wyatt, 2003). But combined with other CBT-i strategies, it provides a supportive foundation.
Maya’s Example
Maya’s evenings often ended with checking emails in bed. We worked on setting a “digital sunset” at 10:00 p.m., shifting her focus to quiet activities instead. This small change reduced stimulation and gave her brain space to settle.
5. Relaxation Training
What It Is
Techniques such as progressive muscle relaxation, deep breathing, or guided imagery reduce physiological arousal—the racing heart and tense muscles that often accompany insomnia.
Research Insight
Relaxation techniques have been shown to decrease pre-sleep arousal and shorten sleep onset latency (Morin et al., 2006).
Maya’s Example
We introduced a 10-minute progressive muscle relaxation exercise before bed. At first, she felt restless, but soon she noticed her body releasing the “wired but tired” energy that had kept her awake.
6. Consistent Wake Times
What It Is
While many people focus on bedtime, wake time is the real anchor for your circadian rhythm. Waking up at the same time every day (including weekends) stabilizes your body clock and strengthens sleep drive.
Research Insight
Consistency in wake times has been linked with improvements in sleep quality, mood, and even metabolic health (Hirshkowitz et al., 2015).
Maya’s Example
Initially, Maya caught up on weekends by sleeping in until 10:00 a.m. We shifted her to a consistent 6:30 a.m. wake time—even on Saturdays. After a few weeks, she noticed she was falling asleep faster during the week.
7. Creating a Strong Sleep Environment
What It Is
Optimizing your bedroom for sleep cues your brain that it’s time to power down. This includes reducing light, keeping the temperature cool, and minimizing noise.
Research Insight
Studies show that environmental factors like light and noise significantly impact sleep architecture, particularly deep (slow-wave) sleep (Basner & McGuire, 2018).
Maya’s Example
Maya invested in blackout curtains and a white-noise machine. These simple adjustments reduced nighttime awakenings and gave her a sense of control over her environment.
Putting It All Together
CBT-i isn’t about quick hacks—it’s about rewiring how your brain and body relate to sleep. For Maya, combining these seven techniques brought steady improvement. After eight weeks, she was falling asleep within 20 minutes, averaging 7 hours of rest, and reporting sharper focus at work.
The research backs her story: CBT-i has been shown to significantly reduce insomnia severity in both clinical trials and real-world practice, with effects lasting months to years after treatment (Trauer et al., 2015).
If you’ve been struggling like Maya—staring at the ceiling, dreading bedtime, or running on empty through your workdays—know that change is possible. CBT-i is the most effective, research-backed treatment for insomnia, and it works without relying on medication.
If you’re ready to finally take back your nights and restore your energy, I offer CBT-i therapy online across British Columbia and much of Canada. You can book a free 15-minute consultation today to see if this approach is right for you.
References
Basner, M., & McGuire, S. (2018). Interactions of sleep and noise. Sleep Health, 4(4), 383-389.
Bootzin, R. R. (1972). Stimulus control treatment for insomnia. Proceedings of the American Psychological Association, 7, 395-396.
Harvey, A. G., Sharpley, A. L., Ree, M. J., Stinson, K., & Clark, D. M. (2011). An open trial of cognitive therapy for chronic insomnia. Behaviour Research and Therapy, 49(6–7), 379-385.
Hirshkowitz, M., et al. (2015). National Sleep Foundation’s sleep time duration recommendations. Sleep Health, 1(1), 40-43.
Kyle, S. D., et al. (2014). Sleep restriction therapy for insomnia is associated with reduced objective total sleep time, increased daytime somnolence, and greater sleep pressure. Sleep, 37(2), 311-317.
Morin, C. M., et al. (2006). Psychological and behavioral treatment of insomnia: Update of the recent evidence (1998–2004). Sleep, 29(11), 1398-1414.
Morin, C. M., et al. (2021). Insomnia disorder. Nature Reviews Disease Primers, 7(1), 55.
Stepanski, E. J., & Wyatt, J. K. (2003). Use of sleep hygiene in the treatment of insomnia. Sleep Medicine Reviews, 7(3), 215-225.
Trauer, J. M., et al. (2015). Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Annals of Internal Medicine, 163(3), 191-204.